Pre-Conditions for the Growth of Addiction
The United States is currently facing a significant drug addiction crisis, with approximately 48.4 million people aged 12 or older having a substance use disorder (SUD) in the past year as of 2024. Among these, opioid addiction remains a critical issue, exacerbated by the rise in synthetic opioids, while marijuana use has also increased, with 22.3% of Americans aged 12 or older reporting use in the past year. The crisis encompasses opioid, marijuana, and other illicit drug addictions, creating widespread societal challenges.
The drug addiction crisis was primarily fueled by several interrelated factors including the over-prescription of opioids in earlier decades, leading to widespread dependency; the infiltration of highly potent synthetic opioids like fentanyl into the drug market; and the increasing social acceptance and legalization of marijuana, which has contributed to higher usage rates. Economic stressors, mental health issues, and gaps in access to effective treatment further accelerated addiction spread. Additionally, illicit drug trafficking has grown in sophistication, increasing availability and risk of overdose.
Social and Economic Impacts
The opioid and broader drug crises place immense strain on healthcare systems. Hospitals experience surges in overdose cases requiring emergency care, intensive treatment, and long-term rehabilitation services. This demand inflates healthcare costs and occupies critical medical resources. Furthermore, an increased number of neonatal abstinence syndrome cases, related to opioid use during pregnancy, implicate additional pediatric healthcare costs and interventions.
On a societal level, addiction contributes to diminished public safety through increased crime rates tied to drug trafficking and impaired functioning. The workforce suffers as productivity declines due to absenteeism, decreased job performance, and rising disability claims related to substance use disorders. Communities face the burden of disrupted families, homelessness, and entrenched cycles of addiction, all of which impede economic development and social cohesion.
Federal Countermeasures
-
Comprehensive Addiction and Recovery Act (CARA) Expansion
This initiative expands funding for prevention, treatment, and recovery programs targeting opioid addiction. It allocates resources to improve access to Medication-Assisted Treatment (MAT) and enhances naloxone distribution to reverse overdoses. CARA also supports educational campaigns and law enforcement training to address both opioid and other substance use disorders effectively.
-
Opioid Crisis Response Act of 2024
Focused on enhancing data collection and opioid prescribing guidelines, this act targets healthcare providers to reduce overprescription. It promotes safe prescribing and integrates prescription drug monitoring programs (PDMPs) nationwide. The act also funds research into non-addictive pain treatments to lessen reliance on opioids.
-
Marijuana Education and Prevention Initiative
This targeted program addresses rising marijuana use, particularly among youth and vulnerable populations. It enhances awareness of marijuana’s effects and potential dependency risks. The initiative collaborates with schools and communities to deliver evidence-based prevention curricula aimed at reducing early onset use and mitigating long-term impact.
-
Enhanced Naloxone Access Act
This action improves the availability and distribution of naloxone kits across all states, including public spaces and first responders. It removes barriers such as prescription requirements and offers training for overdose recognition and response. By increasing naloxone accessibility, it aims to reduce opioid overdose mortality nationwide.
-
Federal Support for State Treatment Infrastructure
Through grants and technical assistance, this measure strengthens state-level treatment programs. It expands facilities offering integrated care for co-occurring mental health and substance use disorders. By fostering interagency cooperation and evidence-based practices, the federal government helps states like Michigan better address addiction treatment needs comprehensively.
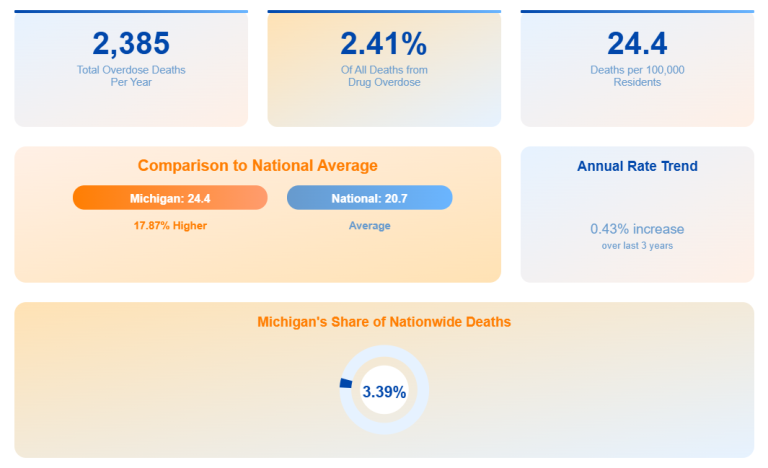
Michigan Case – The Numbers Speak for Themselves
Michigan has experienced a troubling rise in overdose mortality, with over 2,200 deaths annually attributed to opioid and drug overdoses as of 2024. The spread of opioid addiction, including those involving fentanyl, remains high alongside increasing marijuana use disorders. Local authorities have responded by deploying targeted intervention programs, increasing law enforcement training on fentanyl detection, and expanding access to treatment facilities statewide.
| Category | Michigan Data (2024) |
|---|---|
| Annual Overdose Deaths (Opioids & Other Drugs) | 2,200+ |
| Opioid Addiction Rate (%) | ~1.1% |
| Marijuana Use Disorder Prevalence (%) | 6.5% (approx.) |
| Number Receiving Treatment (Opioids & Marijuana) | Estimated 30,000+ annually |
Among Michigan’s state programs, the “Michigan Opioid Partnership and Treatment Expansion” focuses on broadening access to Medication-Assisted Treatment combined with behavioral health services, significantly improving recovery rates through holistic therapy. The “Safe Swaps Program” reduces prescription opioid availability by promoting non-opioid pain management options prescribed by healthcare professionals. Lastly, the “Youth Marijuana Education and Prevention Initiative” delivers targeted school and community programs, aiming to curb rising marijuana use among adolescents and young adults by emphasizing prevention and early intervention.
Approaches in Neighboring Regions
-
Ohio
Ohio implements the “Hub and Spoke” system, which integrates centralized overdose response centers (“hubs”) with local treatment providers (“spokes”). This model ensures continuous care transition from emergency response to long-term treatment, enhancing recovery retention. Ohio reports improved treatment engagement and reduced overdose deaths since implementing this coordinated approach.
-
Indiana
Indiana’s “Law Enforcement Assisted Diversion (LEAD)” program diverts non-violent drug offenders into treatment rather than incarceration. By prioritizing public health over punitive measures, LEAD reduces recidivism and promotes recovery. Participation includes pre-arrest diversion, motivational interviewing, and linkage to community-based services.
-
Wisconsin
Wisconsin’s “Naloxone Access and Education Campaign” combines widespread naloxone distribution with extensive public training and awareness programs. This comprehensive approach empowers communities to reduce opioid-related deaths effectively. It notably includes partnerships with emergency responders, schools, and community organizations to maximize coverage.
Is It Possible to Stop the Crisis? Looking to the Future
-
Investment in Treatment and Recovery Support
Sustained funding for Medication-Assisted Treatment, integrated behavioral health, and recovery housing shows high effectiveness by addressing addiction’s multifaceted nature and reducing relapse rates.
-
Early Intervention and Prevention Programs
Focusing on adolescents and high-risk populations with evidence-based educational campaigns helps prevent initiation and escalation of drug use, particularly marijuana.
-
Interagency Cooperation
Coordination among healthcare, social services, law enforcement, and community organizations enhances holistic response capabilities and reduces gaps in care and enforcement.
-
Decriminalization Coupled with Treatment Access
Decriminalizing minor possession while expanding treatment reduces stigma and encourages individuals to seek help without fear of legal repercussions.
-
Comprehensive Educational Campaigns
Accurate information campaigns targeting misinformation and social normalization of drug use can shift public perception towards understanding addiction as a health issue.
-
Unaccompanied Isolation
Isolating individuals without integrating them into continuous care or community support has proven ineffective and may exacerbate relapse risks.
-
Repressive Measures Alone
Sole reliance on punitive law enforcement without treatment components tends to increase incarceration rates without reducing addiction or overdose deaths.
-
Lack of Aftercare and Support Services
Absence of follow-up care after initial treatment often results in high relapse rates and wasted treatment investments, highlighting aftercare importance.
Conclusions and Recommendations
Addressing the drug crisis is a paramount public health responsibility that demands data-driven, empathetic, and sustained strategies. While each state, including Michigan, implements unique methods, effective responses universally combine reliable data monitoring, open community dialogue, and comprehensive long-term support for those struggling with addiction. Only through such holistic approaches can the epidemic be controlled and lives saved.